Treating ADHD requires a holistic approach which needs to be developed for each individual. It is likely to include a blend of treatments including medical and healthcare treatments, educational and psychological interventions.
These might include medication, parent training and education programmes, psychological support and therapies, occupational therapy and sensory integration, speech and language therapy, behavioural therapy, nutrition and an education about ADHD.
Every child or young person with ADHD is unique and treatment should be tailored to the individual patient. Parents are encouraged to be actively involved in identifying the needs of their children in view of the complexities of the condition and its co-morbidities in order to consider which treatments are the most appropriate. Similarly, parent training for how best to manage children and young people with ADHD is encouraged. Education about ADHD enables parents and teachers to give crucial practical and emotional support.
There is a guide to non-pharmacologic treatments here.
- Medication
- Parent training & Education
- Occupational Therapy & Sensory
- Speech & Language Therapy
- Emotional, Pyschotherapies and CBT
- Nutrition
What do ADHD medications do?
Medication is prescribed to support concentration, reduce hyperactivity, improve impulsivity and help the emotional dysregulation which can characterise ADHD. It may also support improved executive function.
Medication does not cure ADHD – it can only reduce the challenges it causes. It can help to control the core symptoms of ADHD and help children to be more focused and concentrate better. Similarly, due to the complexity of the condition, medication on its own is unlikely to treat ADHD fully.
How does the medication work?
In simple terms, they adjust the levels of dopamine and noradrenaline, two brain chemicals (or neurotransmitters) associated with ADHD. These brain chemicals get released in the spaces between brain cells, and then get carried back into the brain cells by transporters once they have done their job. Once the level of brain chemicals are adjusted, the brain functions more efficiently, and the individual becomes less hyperactive, inattentive, and/or impulsive.
There are two types of medication that can be used either stimulants or non-stimulants.
Watch our useful video which is a 10 minute introduction to Medication with Dr Peter Hill. For a more in-depth and longer discussion on medication refer to the webinar of Dr Maite Ferrin. Dr Peter Hill has also written a recent book “The parents’ guide to ADHD medication”, which can be found here. We also held a webinar with Dr Hill discussing medication more in-depth.
Ben’s story (Aged 11)
“I was always getting into trouble at school. The teacher used to tell me off for not sitting still, I’d try to sit down but it was hard – I would just want to get up and walk around. I was always getting into trouble for talking. The other children in my class would sit still and finish their work but I found this hard. Mum and Dad said I had a lot of energy. Sometimes my friends would tell me I was over the top. Mum says she couldn’t take me anywhere when I was younger because I was so noisy and always on the go. In the end, Mum and Dad took me to a clinic for children who have problems. They said I have ADHD and talked to my parents and teachers about how to help me. They gave me some medication – Ritalin. My Mum and Dad think it helps. I don’t seem to get told off so much and can do my school work better.”
What different medications are used to treat ADHD?
Stimulants:
Methylphenidate is most commonly used in the UK to treat ADHD. Brand names include Medikanet, Ritalin, Equasym, Concerta, Matoride, Delmosart and Xenidate. For children having difficulty swallowing capsules, Medikinet XL and Equasym XL capsules can be carefully opened and the medication inside carefully sprinkled onto something slightly sticky, like a spoonful of yoghurt.
Dexamfetamine (brand names include Dexedrine) is also a stimulant and similar in its actions to methylphenidate. It sometimes works when methylphenidate does not.
Elvanse capsules contain the active ingredient lisdexamfetamine dimesylate. Lisdexamfetamine is converted into dexamfetamine. Lisdexamfetamine capsules can be opened and mixed in with a small amount of water for children who struggle to swallow.
Non-stimulants:
Intuniv is a long-acting form of guanfacine. It is a non-stimulant. It is often prescribed for children who cannot tolerate stimulants, or for parents who prefer not to use stimulants. It’s believed that Intuniv strengthens receptors in the brain, improving memory and attention, reducing distractions, and controlling impulses. It can help reduce symptoms of ADHD.
Atomoxetine is a non- stimulant drug. It is available in liquid form but only on an application to the pharmacy board as an exception.
Combinations of medications are rarely needed, and seldom used. The combination of guanfacine and methylphenidate can be used
There is a limited range of other types of medication that are sometimes used in specialist practice, including Clonidine, certain antidepressants and mood stabilisers.
How long do the benefits of the medication last?
Most of the methylphenidate medications work on improvements lasting from around 4 hours through to around 12 hours, depending on the brand. Lisdexamfetamine lasts around 13 hours. Both guanfacine and atomoxetine take around 6 weeks to show benefits, but once it is effective the benefits last 24 hours. Everyone is different, and some young people do find the medication doesn’t last as long as expected.
With stimulant medications (methylphenidate and lisdexamfetamine) patients often elect not to take medication during weekends or the school holidays and then resume again in school term time. This would usually be to help improve appetite over the weekends / holidays. There are a few young people who do find consistency more helpful who benefit from taking it everyday, including weekends but this would be something to discuss with your doctor.
Are any of the medications for ADHD addictive?
The medication used to treat ADHD are controlled drugs and therefore need to be prescribed as it can impact the individual if other medical conditions (heart conditions or mental health issues) are prevalent. However, the low and steady doses used to treat ADHD do not lead to dependence. Research suggests that children with ADHD are somewhat more likely to use illegal drugs, but that the risk actually falls if they are treated with stimulants. Anecdotal evidence suggests that the use of illegal drugs is more prevalent due to risk-taking nature of ADHD.
The medication has been used over many years and the first Methylphenidate that was licenced in 1955 was Ritalin.
What are the side effects of ADHD medication?
Despite media coverage, side effects for ADHD medication are not usually problematic. The commonest being a loss of appetite. However, your doctor will need to know any side effects your child experiences and they will need to be assessed and managed.
Side effects of stimulant medication for ADHD can include restlessness, difficulty sleeping, irritability and mood swings, depression, loss of appetite, headaches, upset stomach, dizziness, high blood pressure, racing heartbeat and tics. Side effects of non stimulants include restlessness, difficulty sleeping, irritability and mood swings, depression, loss of appetite, headaches, upset stomach, dizziness, low blood pressure and a slowed heartbeat.
Significant side effects typically arise when the selected medication is not suitable to the individual or if the doses is not correct. For these reasons, ADHD medication should only be prescribed to children and young people who have been professionally assessed and diagnosed by an expert, and should be reviewed regularly.
If your child has ADHD, specially tailored parent training and education programmes can help you learn specific ways of talking to your child, and playing and working with them to improve their attention and behaviour.
We run monthly post diagnosis workshops for parents of newly or recently diagnosed children or teenagers. This one-off workshop provides an overview of the condition and is full of essential information that will help you navigate this time of discovery and learning. It is interactive and will allow you to ask question and share ideas. It is also a great opportunity to meet other parents also embarking on the journey with a newly diagnosed child or teen.
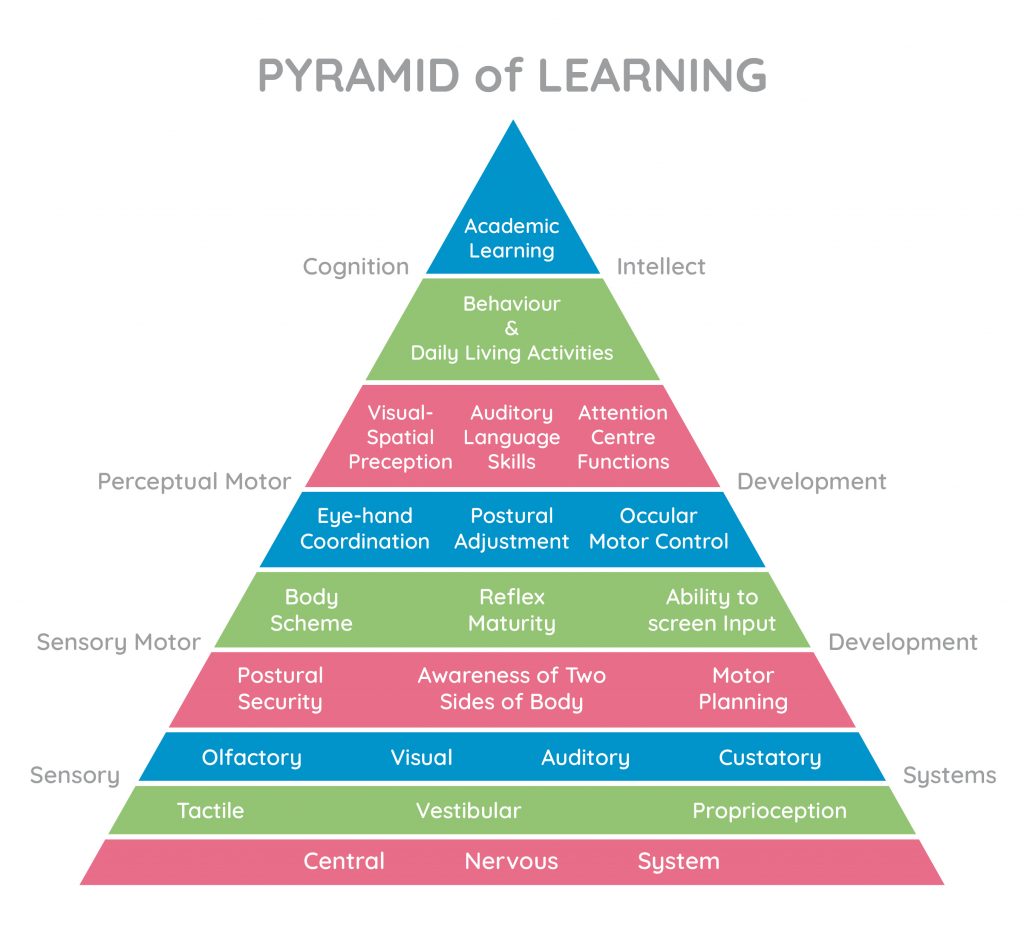
Many children with ADHD experience sensory integration issues, relating to the development of the central nervous system and may have difficulties with one or more of their key senses: auditory (hearing), vestibular (gravity and movement), proprioceptive (muscles and joints), tactile (touch) and visual (seeing). Unless these are developed and supported, it can hugely affect the child or young person’s ability to participate in life at home and school and also to access education. Similarly, if unsupported it can hugely affect the behaviour of the child or young person with ADHD.
Jean Ayres who led pioneering work on sensory integration defined it as:
“The neurological process that organises sensation from one’s own body and from the environment and makes it possible to use the body effectively with the environment”
The pyramid of learning below illustrates the interconnectivity of senses with being able to access learning:
The following checklist by Mel Randall highlights symptoms of sensory integration difficulties a child or young person may experience.
Occupational Therapists specialising in sensory integration will be able to assess your child and develop a programme of support.
Watch our webinar by Occupational Therapist Charlotte O’Reilly on “Building a rich sensory home” [https://adhdembrace.org/our-videos/].
We also have the slides from a talk on Occupational Therapy and ADHD led by Richmond and Kingston Achieving for Children, which are a good resource. For a more detailed, specific exercises, please look here.
Occupational therapy is available on the NHS and a referral can be accessed through Achieving for Children’s Single Point of Access on 020 8547 5008 or for a list of Occupational Therapists with Sensory Integration training visit the following link: . Also Maximum Potential is a specialist practice focused on Sensory Integration. https://maximumpotential.org.uk/
To learn more about sensory integration, a good read is The Out of Sync Child by Carol Kranowitz.
Children and teens with ADHD often have social communication difficulties in that they may find they picking up on social clues or waiting their turn to speak difficult. These are all areas that will affect their ability to build friendships and if not supported the children and teens may find they are socially isolated. Speech and Language Therapy can help children and young people with ADHD by teaching them about attention and listening; coping with instructions; communicating appropriate for their age; social interaction and play.
Social Communication Assessment Team (SCAT) provides a service for children who have social communication difficulties and who may also have unusual patterns of behaviour.
If you want to go private, find a SLT practitioner here.
Behaviour therapies and emotional help should support a child who may as a result of their other challenges of ADHD display behavioural issues or emotional difficulties such as anxiety or depression. These should be put in place in conjunction with ensuring the child is properly supported on their primary needs such as medication for concentration, sensory integration support or social communication.
Behaviour therapies and emotional help provides support for children and young people with ADHD and may involve teachers as well as parents. Behaviour therapy usually involves behaviour management, which uses a system of rewards to encourage a child or teenager’s reaction behaviourally or emotionally to the difficulty experienced with their ADHD.
If your child has ADHD, you can identify types of behaviour you want to encourage, such as sitting at the table to eat or not lashing out at a sibling. The focus of the therapy is to give positive reinforcement or rewards for good behaviour or emotional reactions. Children and teens with ADHD do not always respond well to strict discipline or detentions but operate better if they have clear parameters in which they need to function. The parameters need to be set appropriately so that they are able to comply and so does require reasonable adjustment for their ADHD presentation.
CBT (Cognitive Behaviour Therapy) is a type of talking therapy that attempts to change how people think (cognitive) and what they do (behavioural). CBT can be sought for serious anxiety, depression, sleeping issues connected to ADHD.
The Emotional Health Service through the NHS offers an early response to children and young people experiencing poor emotional well-being and mild-moderate mental health issues. They provide a number of therapies including CBT.
In addition, The Effra Clinic also offer CBT.
Dr Jade Smith’s has written a great book on Adapting CBT for Children with ADHD.
Private Child Psychologists can be found here: http://www.achippp.org.uk/directory
Private Psychotherapist can be found here: https://www.psychotherapy.org.uk/find-a-therapist/?
Nutritional Tips for Children and Young People with ADHD
Supporting children and young people with ADHD through nutrition can significantly impact their behavior, focus, and overall well-being. Good nutrition can have such an impact on individuals with ADHD that we have done several in-depth webinars here. Additionally, here are some key dietary strategies to consider:
1. Start the Day with a Balanced Breakfast
A healthy, nutrient-rich breakfast is crucial for fueling the brain and setting the tone for the day. Foods that combine protein and complex carbohydrates are ideal, as they help the body produce neurotransmitters—the brain’s chemical messengers. Try options like:
- Whole-grain toast with eggs or nut butter
- Greek yogurt with berries and a sprinkle of nuts or seeds
- A smoothie made with spinach, banana, and protein powder
These choices provide sustained energy and prevent mid-morning crashes, helping your child stay alert and focused at school.
2. Balance Blood Sugar Levels
Avoiding sugary and highly processed foods is essential. These can cause spikes and crashes in blood sugar, which may exacerbate hyperactivity and attention difficulties. Instead, prioritize protein-rich foods like:
- Lean meats (chicken, turkey)
- Beans and lentils
- Nuts and seeds
Protein helps stabilize blood sugar levels and supports the production of neurotransmitters, promoting better mood regulation and focus.
3. Include Omega-3 Fatty Acids
Omega-3 fatty acids are essential for healthy brain function, yet the body cannot produce them—they must come from the diet. Studies suggest that children with ADHD often have lower levels of omega-3s than their peers, and increasing intake can improve symptoms like hyperactivity, impulsivity, and concentration.
Good sources of omega-3s include:
- Fatty fish (salmon, mackerel, sardines)
- Walnuts
- Chia seeds and flaxseeds
Alternatively, high-quality fish oil supplements can be a helpful addition to your child’s routine. Consult your healthcare provider before starting any supplements.
4. Avoid Hyperactivity Triggers
Some artificial additives, such as certain colorants and preservatives, are known to increase hyperactivity in children—whether or not they have ADHD. To minimize this risk:
- Swap sweets and processed snacks for fresh, whole-food alternatives like fruit, vegetable sticks, or plain popcorn.
- Read ingredient labels carefully and avoid products with artificial dyes.
5. Identify Food Intolerances and Sensitivities
Food intolerances can sometimes worsen ADHD symptoms. Watch for signs like stomach aches, lethargy, or heightened hyperactivity after eating certain foods. Keeping a food diary can help you identify potential triggers.
If you suspect food intolerances, consider consulting a professional for guidance. The following resources can connect you with qualified practitioners:
- The Association for Nutrition (AfN) provides a directory of Registered Nutritionists who can offer evidence-based advice on diet and health.
- The British Dietetic Association (BDA) can help you find registered dietitians with expertise in supporting children and young people with ADHD.
- The British Association for Nutrition and Lifestyle Medicine (BANT) offers a search tool to locate nutrition professionals.
Conclusion
By focusing on balanced meals, avoiding potential triggers, and incorporating brain-supportive nutrients, you can help manage ADHD symptoms, support your child’s development and improve overall health. Small, sustainable changes in diet can have a meaningful impact over time. Finally, a great recipe resource can be found here: https://www.bda.uk.com/
